If I Have Amerigroup Insurance Will My Baby?
Montana Medicaid and HMK Plus are healthcare benefits for eligible low-income Montanans. Montana Medicaid and HMK Plus pays for services that are:
- Medically necessary,
- Provided by a Montana Medicaid/HMK Plus enrolled provider, and
- Medicaid/HMK Plus covered services.
Announcements
Member Education (Newsletters, Presentations, and Changes to Benefits & Copayments)
Are you eligible?
- Use for healthcare coverage now.
- Contact the Offices of Public Help (OPA) for questions about applications and/or eligibility at ane-888-706-1535.
- Email for a PDF awarding
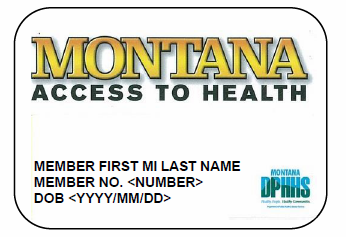
Montana Medicaid and HMK Plus Fellow member Data
Passport to Health (Passport): Choose your chief care provider
Passport is the chief care case management (PCCM) plan for Montana Medicaid and HMK Plus members. The Passport programs back up Medicaid and HMK Plus members, equally well equally, providers to establish a strong physician/patient human relationship and ensure the appropriate use of services.
- Yous can cull your Passport provider anytime online.
- If you practise not cull a Passport provider, you will be assigned one.
- If you need help choosing your Passport provider or have questions regarding Passport, call the Medicaid/HMK Plus Member Help Line at 1-800-362-8312, K-F, 8am-5pm.
- Recall, you volition demand a referral (approval) from your Passport provider before you can see well-nigh other healthcare providers.
- For more Passport information, see the Passport Section of the Member Guide.
Effective for all claims paid on or after January i, 2020 copayments will not be assessed.
What are the Benefits?
Standard Benefits
- Dental care,
- Doctor, hospital, and emergency services,
- Family planning,
- Home health services,
- Laboratory and x-ray services,
- Motherhood and newborn care,
- Mental wellness and substance abuse handling,
- Nurse Beginning Advice Line,
- Prescription drugs,
- Rehabilitative services and supplies,
- School-based services,
- Oral communication therapy, audiology, and hearing aids,
- Transportation to appointments, and
- Vision care.
Adult Dental Benefits
- Preventative (cleaning, fluoride), and
- Anesthesia/sedation services.
In add-on to the benefits above, the post-obit treatment services will also be bachelor, subject to an annual cap of $1,125. Members excluded from this annual cap are: age 20 and nether and members categorically anile, blind, or disabled. Notwithstanding, service limits may apply. The benefit year runs from July 1 through June 30. Y'all volition have to pay for services that are not covered and for those services that go over the $1,125 dental treatment limit for the post-obit listing of treatments:
- Restorative (fillings, crowns),
- Periodontal (glue disease issues), and
- Oral surgery (extractions).
Vision
- Annual exam every two years, and
- Eyeglasses/eyewear every two years (depending on alter in the prescription).
Prescription Drugs
Many prescription drugs are covered. Some prescription drugs may need prior authority. To notice out if a drug you need is covered or to notice out if a drug needs prior authorisation, talk to your chemist or the person who prescribed the drug.
Medicaid will pay for a 34-24-hour interval supply of drugs. Members may get a ninety-24-hour interval supply of some drugs at the time for eye disease, high blood force per unit area, or birth control. Early on refills may exist authorized if the person who writes the prescription changes your dose. Early refills cannot be granted for lost or stolen medication, or for vacation or travel.
Prescription drugs are only covered if you go to a Medicaid-enrolled pharmacy.
Fellow member Rights and Responsibilities
Missed or Canceled Appointments
When members do not testify up for a scheduled appointment, it creates an unused appointment slot that could have been used for another member. Information technology is very important to keep appointments and call the provider in advance if you cannot arrive to a scheduled appointment. Medicaid providers cannot neb a member for no-show/missed appointments. However, a provider may discharge a fellow member from their practice later and then many no-show/missed appointments. The provider must have the same policy for Medicaid members as not-Medicaid members, and must notify Medicaid members that the policy exists.
For a full listing of member rights and responsibilities, see the Member Rights and Responsibilities Section of the Member Guide
Do you still have questions?
Here is a copy of the Montana Medicaid and Healthy Montana Kids Member Guide. Be sure to bank check the announcements section above for information on changes to your benefits.
Member Guide effective one/1/2020
Member Resources
Need help finding your local Office of Public Assistance, Enrolled Medicaid Provider, or Passport Provider? Phone call Montana Healthcare Programs, Fellow member Help Line 1-800-362-8312, G-F, 8am-5pm, for assist.
Find a Montana Medicaid Provider.
Choose a Passport Provider.
Notice a Montana Medicaid or HMK Plus Dental Provider.
Report a alter for your example or use for healthcare coverage.
View details about your case.
I lost my Medicaid/HMK Plus Card, call i-888-706-1535 for a replacement.
Important Contact Numbers
Public Assistance Aid Line
Eligibility and reporting changes to your instance
1-888-706-1535
Medicaid/HMK Plus, Member Aid Line
Medical Benefits, copayments, and Passport to Health questions
one-800-362-8312
Nurse Beginning Communication Line
Talk to a nurse 24 hours a day, 7 days a week
1-800-330-7847
Medicaid Transportation Services
Contact the Medicaid Transportation Center
ane-800-292-7114
Source: https://dphhs.mt.gov/montanahealthcareprograms/memberservices
0 Response to "If I Have Amerigroup Insurance Will My Baby?"
Post a Comment